| IN BRIEF | |
| Registration No.: | XXXX41 |
| Education: | BDS, MDS |
| Experience: | 10 years |
| Languages Known: | English & hindi |
| Activities & Honours | |
| Certifications - 2019: | Office of Diversity & Inclusion Physician Award |
| Awards & Honors - 2019: | Office of Diversity & Inclusion Team Award |
| Professional Memberships | |
| 2022: | Participant: WHO Classification of Tumors of the Eye - 5th Edition - Consensus Group, |
| 2021: | Present Diversity, Equity, and Inclusion Leadership Forum Member |
| 2018: | Present Program Director |
| Department: | Ophthalmology |
| Speciality Groups: | |
| Location: | ABC Hospital, Shankarpur Colony, Bakshi Bazar |
Scaling: Scaling removes tartar and bacteria from your tooth surfaces and below your gumline. It may be done using instruments, a laser or an ultrasonic device.
Root planing: Root planing smooths the root surfaces. This helps prevent further buildup of tartar and bacteria. It also helps your gums attach to your teeth again.
Antibiotics: Topical or oral antibiotics can help control bacterial infection. Topical antibiotics can include antibiotic mouth rinses or putting gel containing an antibiotic into gum pockets. Sometimes oral antibiotics are needed to get of bacteria that cause infections.
To tell whether you have periodontitis and how severe it is, your dentist may:
Review your medical history to identify any factors that could be linked to your symptoms. Examples include smoking or taking certain medicines that cause dry mouth.
Examine your mouth to look for plaque and tartar buildup and check for easy bleeding.
# Measure how deep the pockets are between your gums and teeth by placing a tiny ruler called a dental probe between your teeth and gumline. Pockets are measured at several places in your upper and lower gums. In a healthy mouth, the pocket depth is usually between 1 and 3 millimeters (mm). Pockets deeper than 4 mm may indicate periodontitis. Pockets deeper than 5 mm cannot be cleaned well with routine care.
# Take dental X-rays to check for bone loss in areas where your dentist sees deeper pockets.
# Your dentist may assign a stage and a grade to periodontitis based on how severe the disease is, the complexity of treatment, your risk factors and your health. Then a treatment plan is made.
Treatment: Treatment may be done by a dentist or a periodontist. A periodontist is a dentist who specializes in gum disease. A dental hygienist may work with your dentist or periodontist as part of your treatment plan. The goal of treatment is to thoroughly clean the pockets around teeth and prevent damage to surrounding gum tissue and bone. You have the best chance for successful treatment when you also have a daily routine of good oral care, manage health conditions that may impact dental health and stop tobacco use.
Nonsurgical treatments: If periodontitis isn't advanced, treatment may involve less invasive procedures, including:
# Scaling. Scaling removes tartar and bacteria from your tooth surfaces and below your gumline. It may be done using instruments, a laser or an ultrasonic device.
# Root planing. Root planing smooths the root surfaces. This helps prevent further buildup of tartar and bacteria. It also helps your gums attach to your teeth again.
# Antibiotics. Topical or oral antibiotics can help control bacterial infection. Topical antibiotics can include antibiotic mouth rinses or putting gel containing an antibiotic into gum pockets. Sometimes oral antibiotics are needed to get of bacteria that cause infections.
Surgical treatments: If you have advanced periodontitis, you may need dental surgery, such as:# Flap surgery, also called pocket reduction surgery. Your periodontist makes cuts in your gums to carefully fold back the tissue. This exposes the tooth roots for more effective scaling and root planing. Because periodontitis often causes bone loss, the underlying bone may be reshaped before the gum tissue is stitched back in place. After you heal, it's easier to clean the areas around your teeth and maintain healthy gum tissue.
# Soft tissue grafts. When you lose gum tissue, your gumline gets lower, exposing some of your tooth roots. You may need to have some of the damaged tissue reinforced. This is usually done by removing a small amount of tissue from the roof of your mouth or using tissue from another donor source and attaching it to the affected site. This can help reduce further gum loss, cover exposed roots and give your teeth a better appearance.
# Bone grafting. This procedure is performed when periodontitis destroys the bone around your tooth root. The graft may be made from small bits of your own bone, or the bone may be made of artificial material or donated. The bone graft helps prevent tooth loss by holding your tooth in place. It also serves as a platform for the regrowth of natural bone.
# Guided tissue regeneration. This allows the regrowth of bone that was destroyed by bacteria. In one approach, your dentist places a special type of fabric between existing bone and your tooth. The material prevents unwanted tissue from growing into the healing area, allowing bone to grow back instead.
# Tissue-stimulating proteins. Another approach involves applying a special gel to a diseased tooth root. This gel contains the same proteins found in developing tooth enamel and stimulates the growth of healthy bone and tissue.
Flap surgery, also called pocket reduction surgery: Your periodontist makes cuts in your gums to carefully fold back the tissue. This exposes the tooth roots for more effective scaling and root planing. Because periodontitis often causes bone loss, the underlying bone may be reshaped before the gum tissue is stitched back in place. After you heal, it's easier to clean the areas around your teeth and maintain healthy gum tissue.
Soft tissue grafts: When you lose gum tissue, your gumline gets lower, exposing some of your tooth roots. You may need to have some of the damaged tissue reinforced. This is usually done by removing a small amount of tissue from the roof of your mouth or using tissue from another donor source and attaching it to the affected site. This can help reduce further gum loss, cover exposed roots and give your teeth a better appearance.
Bone grafting: This procedure is performed when periodontitis destroys the bone around your tooth root. The graft may be made from small bits of your own bone, or the bone may be made of artificial material or donated. The bone graft helps prevent tooth loss by holding your tooth in place. It also serves as a platform for the regrowth of natural bone.
Guided tissue regeneration: This allows the regrowth of bone that was destroyed by bacteria. In one approach, your dentist places a special type of fabric between existing bone and your tooth. The material prevents unwanted tissue from growing into the healing area, allowing bone to grow back instead.
Tissue-stimulating proteins: Another approach involves applying a special gel to a diseased tooth root. This gel contains the same proteins found in developing tooth enamel and stimulates the growth of healthy bone and tissue.
Type here your biography
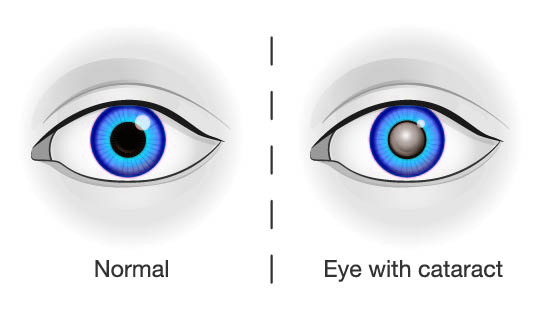
CATARACT
How does a cataract eye look like?
What are the most common types of cataracts?
Some of the most common forms of cataracts are age-related cataracts. Age-related cataracts occur when the proteins in the eye’s lens start to clump together. This causes the lens to become cloudy and makes it difficult to see clearly.
Age-related cataracts are not preventable, but they are treatable. Surgery is the only way to remove a cataract. During surgery, an ophthalmologist will make an incision in the eye and then use a special instrument to break up the cloudy lens and remove it. A new artificial lens will be inserted in its place. Surgery is usually successful in improving vision and can be performed on an outpatient basis.
The age-related cataracts are termed subject to their location as below:
- Nuclear Cataracts – The cataracts appear in the centre of the lens is known as nuclear cataracts. These may cause double vision or even multiple copies of an image.
- Cortical Cataracts - The cataracts are the ones that affect the edges of the lens, and work their way inward. You may notice white coloration around the lens that gradually increases as it grows in size and moves inward. These cause problems with glare.
- Posterior Sub-Capsular Cataracts - The cataracts occur on the back of the lens are recorded as posterior sub-capsular cataracts. These reduce your ability to read, even in bright light. This type of cataract may cause glare or halos around lights at night.
The additional classes of cataracts are grouped according to their causes as below:
- Secondary cataracts – These secondary cataracts sometimes form because of a chronic illness such as diabetes, after surgery for other eye problems, or from long-term steroid use.
- Traumatic cataracts – The traumatic cataracts result from an eye injury.
- Radiation cataracts – The radiation cataracts may occur after severe exposure to ionizing radiation.
- Congenital cataracts – This type of cataracts appear in new-borns babies or in childhood. They may be caused by a genetic mutation or because of an illness in the mother during pregnancy.
What are the symptoms of cataracts?
The following are the signs or symptoms of cataracts that you could experience:
- Clouded, blurred or dim vision.
- Poor night vision or increased difficulty seeing in the dark.
- Lamps, sunlight, or headlights seeming too bright.
- A halo effect around lights.
- Trouble seeing at night.
- Need for brighter light for reading and other activities.
- Regular changes in eyeglass or contact lens prescription.
- Faded or yellowing colours
- Double vision or multiple images in the affected eye (this symptom may disappear as the cataract grows)
However, in some people, they may not experience any symptoms or signs of cataract until the cataract is well formed, and then they notice a change in their vision.
What are the causes of cataracts?
Aging is the most common cause of cataracts. Also, many conditions and habits make cataracts more likely to develop because of:
- Diabetes
- Alcohol use
- Too much exposure to sunlight
- Smoking
- Inadequate vitamin intake
- Long-term steroid use
- High Blood Pressure
- Previous Eye Problems/Surgeries
- Family History
- Obesity
- Diet high in carbohydrates
Are cataracts painful?
Cataracts don’t usually hurt. But they can cause discomfort by making your eyes more sensitive to light.
How are cataracts diagnosed?
To find out if you have cataracts, your doctor would want to know all about your symptoms. They’ll look closely at your eyes and may do some tests including:
- Visual acuity test: This is a fancy way of saying "eye chart exam." Your doctor will ask you to read letters from a distance to find out how sharp your vision is. First, you'll try it with one eye and then the other. They may also then do a glare test, where they shine a bright light in your eye and then ask you to read the letters.
- Slit-lamp exam: This uses a special microscope with a bright light that lets your doctor check different parts of your eye. They'll look at your cornea, the clear outer layer. They'll also examine the iris -- the colored part of your eye -- and the lens that sits behind it. The lens bends light as it enters your eye so you can see things clearly.
- Retinal exam: Your doctor puts drops in your eyes to widen your pupils, the dark spots in the middle that control how much light gets in. This lets them get a good look at the retina -- the tissue around the back of your eyes -- and a better view of the cataract.
What’s the Treatment?
Surgery is the only way to treat cataracts, but you may not need it right away. If you catch the problem at an early stage, you might be able to get by with a new prescription for your glasses. A stronger lens can make your vision better for a while.
If you have trouble reading, try a brighter lamp or a magnifying glass. If glare is a problem for you, check out special glasses that have an anti-glare coating. They can help when you drive at night.
Keep close tabs on how your cataracts affect the way you see. When your vision troubles start to get in the way of your daily routine -- especially if they make driving dangerous -- it's time to talk to your doctor about surgery.
Cataract surgery
There are several kinds of operations for cataracts, but they all have one thing in common: Your surgeon takes out the cloudy lens and replaces it with an artificial one.
You might feel a little uncomfortable with the idea of an operation on a sensitive spot like your eye. But it's a very common procedure. You'll get medicine called local anesthesia to numb your eye. You’ll be awake but sedated, and you won't feel anything.
It usually takes about 15 to 20 minutes, and you don't need to stay overnight in a hospital. If you have cataracts in both eyes, your doctor will wait until your first eye heals before they perform surgery on the second. More than 95% of people who have this done say they can see better afterward.
- Small-incision surgery. You may also hear your doctor call this phacoemulsification. Your surgeon makes a tiny cut on your cornea. They put a small device in your eye that gives off ultrasound waves that break up your cloudy lens. Then, they take out the pieces and put in the artificial lens.
- Large-incision surgery. This isn’t done as often, but doctors sometimes suggest it for larger cataracts that cause more vision trouble than usual. It's sometimes called extracapsular cataract extraction. Your surgeon takes out your clouded lens in one piece and swaps it out for an artificial one. You'll probably need a little more time to heal from this surgery than from the small-incision type.
- Femtosecond laser surgery. In this operation, your surgeon uses a laser to break up the lens. As with the other types, they'll then put in the new lens. Your doctor may suggest this if you also have an astigmatism, a curve of your cornea that makes your vision blurry. Your surgeon can treat that problem during the cataract surgery by using the laser to reshape your cornea.
Can cataracts be prevented from becoming worse?
In general, prevention is difficult because there is no scientific proof that you can prevent cataracts from getting worse, but the most helpful practice to reduce your risk factors is to:
- Avoid Ultraviolet Light: Prolonged exposure to ultraviolet light from the sun with sunglasses especially in the peak hours of the day for sun exposure are between 10am and 3pm, or 11am and 4pm during daylight savings time.
- Avoid Steroid Eye Drops - Steroid eye drops used to treat dry eyes and arthritic flare-ups in the eyes. Prolonged steroid eye drop use can lead to faster cataract formation in the affected eye. These steroids may be necessary for another eye condition, so schedule regular visits with an ophthalmologist to keep cataracts in check.
- Control Diabetes – Studies suggest that those with diabetes are at greater risk for developing cataracts. Your lens swells if your blood sugar stays too high for too long. Your lens also changes blood sugar into sorbitol. When this substance collects in the lens of your eye, you see less clearly, and a cataract may form. That is why maintaining healthy blood sugar is so important—for both your overall health and the health of your vision.
- Limit Alcohol Consumption – Excess alcohol consumption can pose a number of health risks, including an increased chance of developing cataracts. Therefore preferably avoid alcohol consumption completely but if you cannot then enjoy your wine, beer or cocktails in moderation.
- Quit Smoking – Research suggests that smoking doubles your chances of developing cataracts and the risk continues to grow based on how much you smoke.
- Eat a Healthy Diet – A healthy diet should be a priority for all of us. Should eat foods high in antioxidants, such as beta-carotene, selenium and vitamins C and E, because these may help ward off cataract growth. For instance those who follow a diet including colourful fruits, vegetables, and whole grains may show a decreased chance of developing cataracts. Studies suggest that antioxidant vitamins in these fruits and vegetables may reduce the risk of cataracts. Carrots are a great source of beta-carotene, which is converted into vitamin A in the body and is excellent for eye health. The consumption of fish has been linked to a reduced risk of cataracts. Fish are high in omega-3 fatty acids, which has been cited to reduce cataract progression. You may not have heard of lutein and zeaxanthin. These are two more vitamins that could help protect your eyes from cataracts. Eggs have them, as do green, leafy vegetables. Foods that are rich in a variety of vitamins and minerals may delay cataracts.
- Continue Regular Eye Checkups – Even if your vision is clear and healthy, make it a priority to schedule yearly eye exams. Routine visits allow your doctor to look for signs of cataracts, glaucoma, macular degeneration and other vision disorders. Early detection can be key in saving your vision.
Eyeglasses and Contact Lenses for Cataracts
Eyeglasses and contact lenses are not a treatment for cataracts. Cataracts are typically addressed through cataract surgery, during which the cloudy natural lens is removed and replaced with an artificial intraocular lens (IOL). The IOL can be chosen to address refractive errors like near-sightedness, farsightedness, or astigmatism, but the primary goal of cataract surgery is to restore clear vision. Before surgery, your eye doctor may prescribe glasses or contact lenses to improve your vision temporarily. These are not cures for cataracts but aids for managing the condition until surgery is considered. Consult with an eye care professional for guidance on your specific situation and potential IOL options.
Disclaimer
The content of this article is from various medical information, compiled for you to be alert as a knowledge base information and not as a medical or clinical advice. Therefore do not use this article for self-medication or any other purpose or purposes. The contents of all our articles or posts in any media are just for notification as a precautionary measure. We strictly encourage you to consult your health care providers (doctor, registered dietitian, pharmacist, etc.) for any medication or any other medical or clinical advice or treatments in the best interest of your inclusive health. Any mention in this publication of a specific product or service, or recommendation from an organization or professional society, does not represent an endorsement by srsphysicians.com, Inc. or its affiliates of that product, service, or expert advice.
You may start by seeing your general dentist. Depending on how severe your periodontitis is, your dentist may refer you to a specialist in the treatment of periodontal disease called a periodontist.
Here's some information to help you get ready for your appointment.
What you can do Before your appointment, make a list of:
- Any symptoms you're experiencing, including any that may not seem related to the reason for your appointment.
- Key personal information, such as any medical conditions you may have.
- All medicines you take, including over-the-counter medicines, vitamins, herbs or other supplements, and the doses.
- Questions to ask your dentist.
Questions to ask your dentist may include:
- What's likely causing my symptoms?
- What kinds of tests, if any, do I need?
- What's the best plan of action?
- Will my dental insurance cover the treatments you're recommending?
- What are other options to the approach you're suggesting?
- Are there any restrictions that I need to follow?
- What steps can I take at home to keep my gums and teeth healthy?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
- Feel free to ask other questions during your appointment.
What to expect from your dentist Your dentist may ask you questions, such as:
- When did you first start having symptoms?
- Do you have symptoms all the time or do they come and go?
- How often do you brush your teeth?
- Do you use dental floss? How often?
- How often do you see a dentist?
- What medical conditions do you have?
- What medicines do you take?
- Do you use tobacco products?
Preparing for questions will help you make the most of your time with the dentist.
Address:
TVK Residency,
Banjara Hills, Hyderabad-500034
Email: [email protected]
Phone number: +916309621912 +916309621913 +916309621914
(call is free)
Site visits: 10 am — 6 pm (Monday to Sunday)
Location link: https://maps.app.goo.gl/B4KKUp...
How to Reach Us
We are located in the off road diagonally opposite to TV 9. The lane before chutneys. Walk 200 meters and turn right. Now go down the street until you see the dead end and it is on your LHS.
Here, pl type your Admin / Customer Care No.
No reviews found




